We live in a story that originates in our autonomic state, is sent through autonomic pathways from the body to the brain, and is then translated by the brain into the beliefs that guide our daily living. The mind narrates what the nervous system knows. Story follows state. (The Polyvagal Theory in Therapy, p. 35)
We are immersed in stories. There are the narratives we trade in conversation, the cultural myths that unite and divide us, the fictions we suspend disbelief for, the silent tales we tell ourselves about who we are. Stories disguise, reveal, constrain, bias, entertain, and enlighten us. They shape our lives and identities.
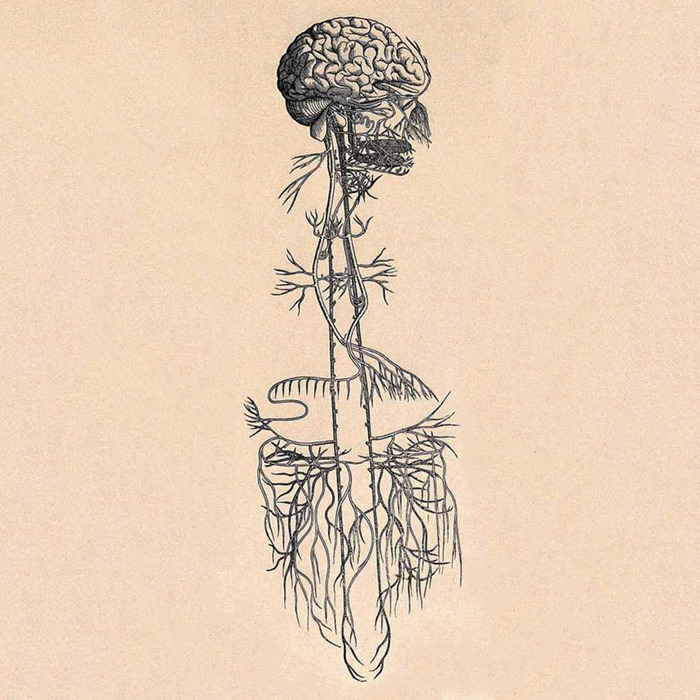
But what shapes story? In her book, The Polyvagal Theory in Therapy, Deb Dana directs us to look beneath story to “the foundation of our lived experience,” the autonomic nervous system (ANS). Merging the neuroscience research of Stephen Porges with her own clinical wisdom, she urges us to befriend our nervous systems, to learn what different levels of ANS activation feel like, and to notice how our stories change depending on what is happening inside our bodies.
Both in the book and at her recent workshop sponsored by CCIH, Deb starts us off on this autonomic exploration with the Personal Profile Map. The map uses a ladder as a visual metaphor for the ANS, which travels more or less vertically through the body, connecting head and heart and belly. The ladder and the map are divided in thirds to demarcate the three primary pathways of the ANS: ventral vagal at the top, sympathetic in the middle, and dorsal vagal at the bottom.
Although all three of these pathways help to run the biological software that keeps us alive, the equilibrium between them shifts in response to the presence or absence of danger. When our systems detect a threat of any kind, we are likely to be in either a sympathetic- or dorsal vagal-dominant state. When we sense that we are safe, the ventral vagal pathway is dominant.
Ventral vagal is the state associated with physical wellbeing—our breathing and blood pressure are level, our bodies relatively at ease. From this platform of physiological regulation, we experience our greatest capacities for connection and creativity, for curiosity and awe. We live here, at the top of the ladder, when our environments provide sufficient cues of safety for our defenses to relax.
At the first sign of danger—be it physical or emotional, internal or external, actual or perceived—we move down the ladder into sympathetic mobilization. Our felt experience of the sympathetic state ranges from vague unease to persistent anxiety to full-blown terror. This is where our “fight or flight” reflexes originate. Hearts race, muscles tense, thoughts spin, and ventral vagal calm feels more or less out of our reach.
If we are not able to regain safe ground, when either the danger we are faced with is too overwhelming or the sense of threat is too unrelenting, we move further down the ladder into dorsal vagal shutdown. The dorsal vagus offers us the protection of last resort—freeze, or feigned death, an immobilized state in which both pain and fear diminish. In non-life threatening situations, we often associate this state with physical lethargy, collapsed posture, mental fogginess, emotional numbing, and social withdrawal.
By “mapping” our nervous systems, using words and/or images to capture our physical and emotional experience in each autonomic state, we bring conscious awareness to subconscious terrain. State shifts happen automatically, faster than thought—we do not get to choose whether our systems will move us up or down the ladder, toward connection or into defense. But the more we look around and notice where we are, the easier it becomes to trace how we got there. We get better at predicting the triggers that are likely to take us down a few rungs and, with practice, we can begin to make more effective use of the resources that help us to climb back up.
Another awareness comes, too. . .we start to notice that our internal narrator has more than one voice, that each of our stories has many possible perspectives. In dorsal vagal, we might tell a tale of doom, of nothing matters, of nothing ever changes. As we move up the ladder into sympathetic, that same story can take on a new sense of urgency and sometimes wildly unsettling uncertainty.
From here, we could easily tumble back into the tight confines of collapse, where our systems might feel safer and our stories reassume an air of hopeless inevitability. But if we are supported enough and safe enough to reach ventral vagal, the plot twists once again, the scope widens. At the top of our ladders, even if only for a moment, we have the space to rest and the chance to recognize that no story is big enough to contain all that we are.
It might seem that such fundamental changes in perspective would announce themselves loudly, that surely we would detect the shape-shifting of our personal narratives. And there are times when this is true, especially when a dramatic event occurs that moves us along the full length of the ladder: the phone rings, and we get the news we have been dreading; or the phone rings, and all is well, just as we had hoped.
But more often than not, our states shift quite subtly, many times in a day, and the stories we live by are told in whispers. It requires patience and courage to learn and to listen. It takes time and support to notice where we get stuck in our own unique autonomic and narrative loops. Making our way to the top of the ladder, to the place where story can fall away if we let it, doesn’t just happen once, but over and over and over again. It’s the everyday work of a lifetime.